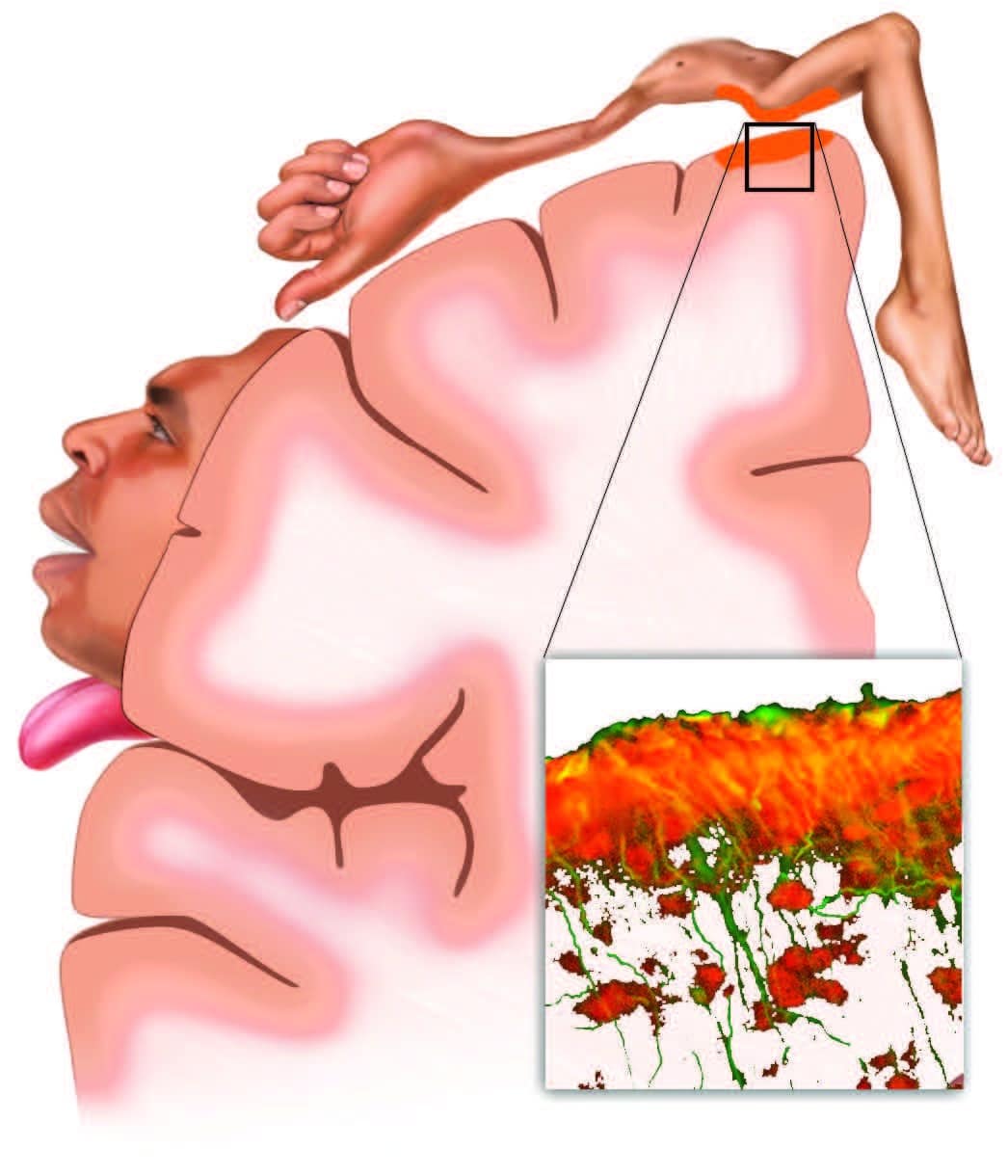
Chances are very good that if you have pain or discomfort, inflammation is to blame; if not wholly, then at least in large part.
Inflammation is directly involved in the pain conditions ranging from sciatica to arthritis, whiplash to tennis elbow, and from migraines to postexercise muscle soreness. So how exactly does inflammation trigger pain?
Pain (like inflammation itself) is biologically and behaviorally necessary. Pain protects against tissue damage by shaping our behavior, while inflammation protects against tissue damage by mobilizing our immune system’s physiological safeguarding and repair functions. Both of these kinds of protection—behavioral and immunological—make sense when danger or damage are actually present; but both pain and inflammation can become problematic when they chronically persist after the threat is no longer around.
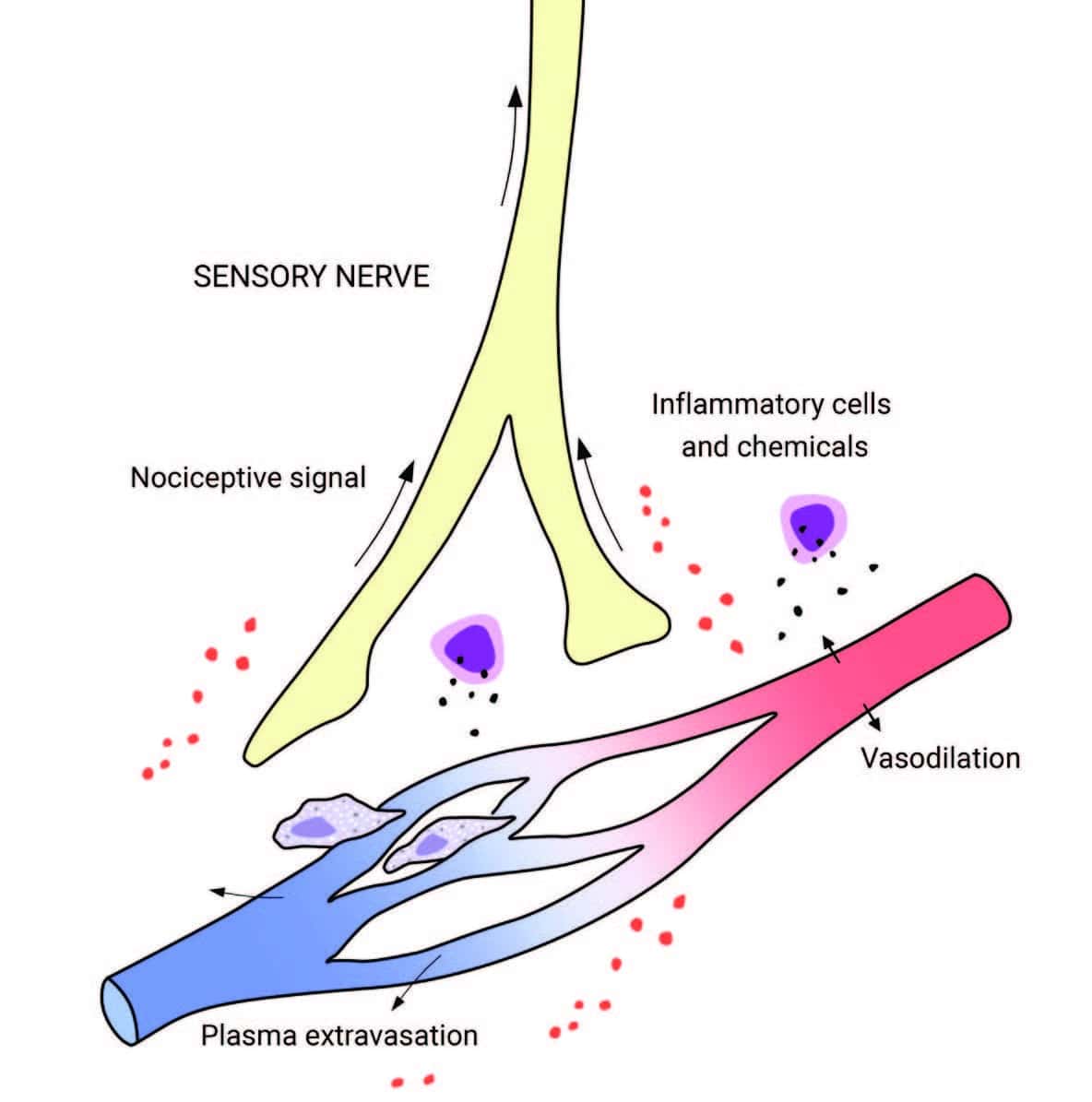
Also, keep in mind that pain and nociception are not the same thing. Nociception is a nerve signal indicating potential mechanical, thermal, or chemical threat to tissues; pain is the experience the nervous system generates in response.
Many times, when your pain is prolonged, it can be because there is continued nociceptive input (for example, from ongoing mechanical or inflammatory irritation). But pain can persist even with little or no tissue damage; or, even when there is obvious damage or degeneration, there can be little or no pain experience at all. And while your pain may not be as related to physical tissue damage as we might have thought, there turns out to be a strong relationship between pain and expectations, fears, context, memory, and social influences.
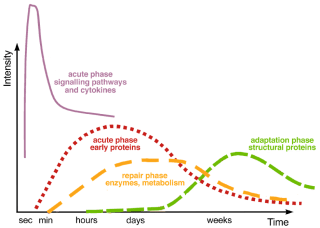
These psychosocial factors play a role in inflammation, as well as in pain. For example, high hostility scores have been correlated with increased inflammation, while openness (hostility’s flip-side) has been associated with decreased inflammatory markers. But the relationship between pain, inflammation, and psychosocial factors is nuanced and complex: while depressed people often have stronger inflammatory responses, turning down inflammation with immunosuppressive drugs can also trigger depressive mood changes. So even though pain, inflammation, and reactive emotions are deeply interconnected, they don’t move in lockstep with one another. Instead, they could be thought of as different modes of physical, psychological, and behavioral adaptation that we use in varying ways in the face of perceived threat.