Have You Been Told You Have a Degenerative Condition, Herniated or Bulging Disc in Your Lumbar Spine?

You’ve had chronic low back pain for months and/or years. Your doctor ordered you an MRI which showed multi-level degeneration/ arthritis, bulging or herniated disk(s), stenosis, or another long terrifying word. You were told you the treatment options were steroid or an epidural injection, NSAIDs, opioids, physiotherapy or even to consult a neurosurgeon. You may have been told that you have to live with this pain. You tried a few of those treatment options with no success or the success (pain relief) was short lived. This left you disheartened, depressed and thinking that you are going to be in pain for the rest of your life. You now avoid physical activity because you think or have been told that it will make your condition worse.
Sound familiar? I hear various versions of this story on a daily basis during my initial consultations. While MRI and other diagnostic imaging remains an excellent assessment tool, it unfortunately carries the burden of giving patients a beautiful mental image of ‘how bad their injury is’ and can contribute to negative thoughts about recovery and prognosis. (Wang et al., 2018)
What if I told you that asymptomatic individuals (people without pain or other symptoms of disease/condition) can have the same CT/ MRI findings as you?
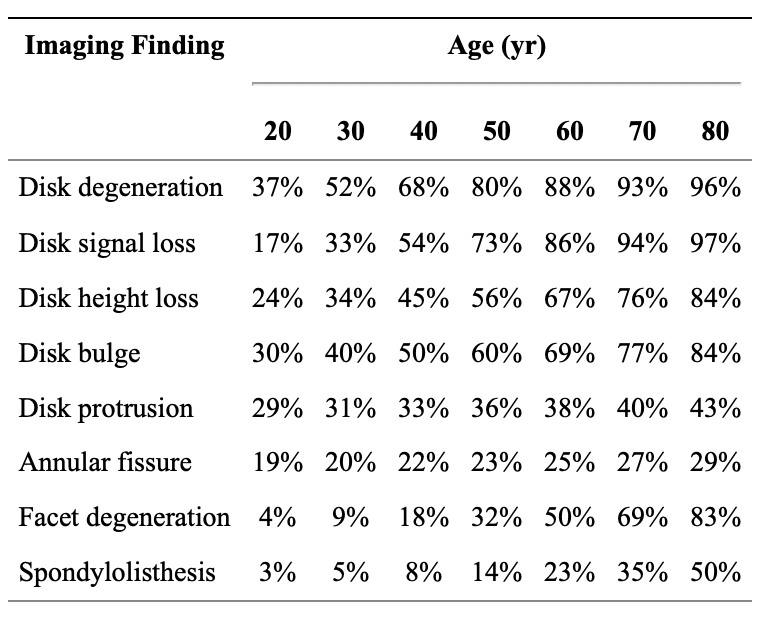
A study conducted by Brinjikji, et al. (2015), systematically reviews the evidence for the prevalence of common spine conditions on asymptomatic people through decades of age: 20, 30, 40, 50, 60, 70, and 80 y/o. The goal of this study was to estimate the prevalence of common spine conditions which showed on diagnostic imaging of healthy individuals (asymptomatic). This study reviewed 33 articles reporting imaging findings for 3110 asymptomatic individuals.
What does this mean for you?
This study proves that some findings are part of the normal aging process and may be unassociated with low back pain. In short, your pain MAY NOT be stemming from what shows up on diagnostic imaging reports! It is our job as your healthcare providers to make a clinical judgement based on our assessments, the patient history and diagnostic imaging to figure out exactly what is MOST LIKELY causing your pain and then discuss your treatment options. In many cases, you DO have conservative treatment options and likewise, the worst thing many patients can do is avoid any type physical activity. Of course, in some circumstances the diagnostic imaging does help us determine the source of your pain, it also helps us better understand what is going on in your spine, what we can expect in terms of recovery, and what is the best available options for your unique circumstance.
We as healthcare practitioners NEED to do a better job of educating the patient about the findings and how they correlate to their pain. We also need to do a better job of not basing a diagnosis solely on diagnostic imaging.
If this sounds like your situation, what should you do?
- Try not to get down on yourself. Being in this situation is NOT your fault.
- Try to avoid Dr. Google. Not everything on the internet is true or is right for your condition.
- Take back control of your health. Schedule a consultation to review your unique case. After our examination and review, we will discuss available treatment options for you and educate you on your condition and what it means for you. For the most part, there are several conservative treatment options available, even if you suffer from failed spinal surgery. (Less than 2% of people with low back pain have potentially serious spine conditions that will require surgery or medical intervention. (Dagenais S, Haldeman S., 2011 and Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. 2009).
Take back control of your health. Schedule a consultation today.
References:
Wáng, Y. X. J., Wu, A. M., Santiago, F. R., & Nogueira-Barbosa, M. H. (2018). Informed appropriate imaging for low back pain management: A narrative review. Journal of orthopaedic translation.
Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis & Rheumatism 2009; 60(10):3072-80.
Dagenais S, Haldeman S. Evidence-based management of low back pain. St Louis (MO): Mosby; 2011;Â p. 1-12.